Photoacoustics: the echo of light
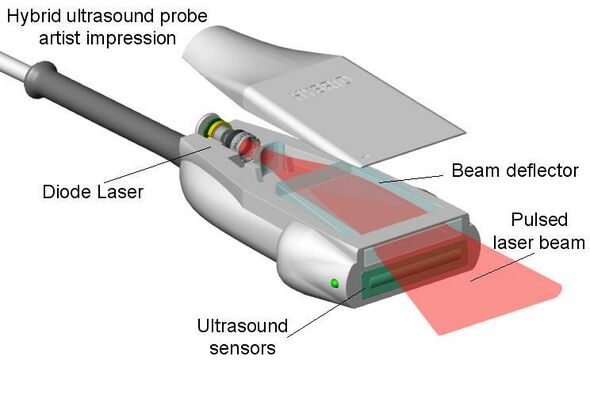
It is light, used to create sound, which is subsequently converted into images: photoacoustics goes beyond the traditional ultrasound scan. The European FULLPHASE project should lead to a handy photoacoustics scanner with an integrated pulsed laser, which can be used to gauge the risk of carotid plaque, for example. The research group at Cardiovascular Mechanics will be checking if it could actually work.
Echography with ultrasound is a widely-used method to map the inner human being – think of ultrasounds used on pregnant women. An ultrasound scanner transmits sound waves the body echoes and scatters. The echo waves are intercepted by the scanner, which thus acts as a sender as well as a receiver. Based on the sound waves, special software reconstructs what’s going on within reach of the scanner.
The technique is fast, relatively cheap, and has no known side effects. Still, there are some downsides to it. For example, ultrasound doesn’t allow for an easy distinction between various tissue types. The difference between water, bone, and soft tissue is clear, but ultrasound isn’t great for distinguishing between tumors and healthy tissue, gauging the nature of carotid plaque, or determining the perfusion of muscle tissue.
In principle, the latter can be done using a related technique: photoacoustics. With this technique, the sound wave in the body that is to be intercepted is provoked with a short laser pulse. “Instead of high-frequency sound, you send a short, intense pulse into the body”, dr.ir. Marcel Rutten explains. “This light is absorbed by, say, blood cells or other particles, depending on the color of light you’re using. Those particles become very hot and expand in no time, after which the surrounding tissue cools them again so they shrink back into shape.” This process creates a sound impulse lasting dozens to up to hundreds of nanoseconds, creating ultrasound with the same frequency – five to ten megahertz – as traditional ultrasound scanners.
Every tissue type responds differently to different light colors. Because of that, it’s possible to specifically heat certain tissues, and have those light up via the ultrasound that’s transmitted. “By playing around with the color of the light, you can decide to visualize oxygenized blood only”, dr.ir. Richard Lopata adds. He has another example: “Diseased blood vessels contain a lot of fat. Photoacoustics are great for finding exactly where that fat is located and how much it is.”
Laboratories have been experimenting with photoacoustics for years, but because of the costs and size of the laser equipment that’s needed, the technique has not made it to hospitals yet. Lopata and Rutten, both assistant professors in the group of Cardiovascular Biomechanics of prof.dr.ir. Frans van de Vosse, are adamant to change that. It’s the reason they’re taking part in a major European project launched last month: FULLPHASE. The project should result in a hand-held photoacoustic scanner that’s easy to use for doctors in hospitals.
The TU/e delegation within the FULLPHASE project are in charge of the ‘preclinical validation’, meaning they’ll be testing the equipment on live tissue as well as compare it to traditional ultrasound scans. Out of the seven-million-euro budget they have been granted more than 800,000 euro for the preclinical validation, which is enough for two doctoral candidates and leaves ample leeway for equipment. On top of that, project leader and manufacturer of ultrasound scanners Esaote made sure they have special scanners at their disposal. Lopata: “These enable us to read raw data, which provides us with more relevant information than the standard images those clinical scanners produce automatically.”
Of course, working with laser pulses has its limitations as well. First of all, light has a hard time penetrating our bodies, even infrared light (ranging from 650 to 1300 nanometers) like that of the scanner. Current lasers can’t go deeper than one centimeter below the skin. “The higher the intensity of the light, the deeper you can peer into the body”, Rutten says. “FULLPHASE wants to get to two centimeters.”
Because of the limited penetration depth, photoacoustics can only visualize tissue that’s located just beneath the skin. Therefore, the FULLPHASE project is studying skin tumors and rheumatic arthritis in phalanges, for example. The Eindhoven researchers are especially looking at perfusion in muscles and carotid plaque. Lopata: “The latter subject is especially relevant. Should plaque tear, the contents – usually fat – end up in the bloodstream and could be transported to the brains, causing a cerebral infarction.”
Rutten even goes so far as to say it’s the holy grail of vascular surgery: “In five out of six cases where plaque is removed from the carotid artery, it turns out the risky operation wasn’t necessary because the plaque was stable. Photacoustics provide a quick and easy way to determine whether or not an operation is needed. It’s much faster and cheaper than an MRI of CT scan, images of which require elaborate interpretation by the doctor at that.
It won’t be easy creating a photoacoustic scanner that’s both handy and safe. Although the average laser power doesn’t have to be that great because of the short pulses, the scanner would still require a powerful power supply to include into the handheld device. Lopata: “There’s a risk of the device overheating and harming the sensitive electronics. Besides, doctors should be able to work with it all day without burning themselves.”
The final problem concerns the high intensity of the laser pulse that’s needed: the heat of the laser could cause burns on the skin. Needless to say, safety is an important issue within the project. Rutten isn’t too confident that final problem can be solved: “Lasers are subject to all kinds of safety regulations, but those were drawn up back when people weren’t fully aware of the effects of pulsed lasers. Because of that they’ve been overly careful, so there’s a risk FULLPHASE either produces a device that can’t be used despite its safety, or the device becoming too safe due to which it loses its clinical use.”


Discussion