Fetus in distress
She was already a medical doctor, but now she’s that other doctor as well. Dr. Judith van Laar researched ways to determine, based on their heart rate, if an unborn child is in danger during the mother’s pregnancy. The gynecologist in training received her doctorate from the Department of Electrical Engineering on October 31.
Whenever a baby’s in trouble in the uterus, doctors may decide to induce labor or do a C-section. These interventions can save the baby’s life, but quite often the procedure turns out to have been unnecessary. It’s a problem, because ‘it doesn’t hurt to try’ doesn’t apply here, especially if the child is born well before their due date. Premature birth is one of the main causes for disease and death with newborns.
Besides, such a traumatic start to life can reverberate for a long time. Especially if paired with oxygen deficiency prognoses can be grim, says Van Laar. Caesarian sections aren’t without risk for mothers, either, she adds. “It’s still abdominal surgery with a risk of internal bleeding, infection and organ damage. And the uterus is scarred, due to which it may tear during a next pregnancy.”
Van Laar is a gynecologist in training at the Máxima Medisch Centrum in Veldhoven. Next to her training, supervised by doctor and TU/e part-time professor prof.dr. Guid Oei, she’s also been conducting scientific research over the past years. She now obtained her doctorate from the Department of Electrical Engineering, supervised by that same Oei. The main goal of Van Laar’s research was to prevent children from suffering from oxygen deficiency or unnecessary premature birth.
To check up on the unborn child during pregnancies, doctors use a cardiotocogram, monitoring both the child’s heart rate and the contraction of the mother’s uterus. Measurements can be done from outside using ultrasound, like the ultrasounds we all know. Still, for an accurate, long-lasting measurement of the baby’s heart rate an electrode should be pasted to the child’s body, which is something that can only really be done when the mother has gone into labor.
“The cardiotocogram is widely used, but turns out to be of limited diagnostic value”, says Van Laar. An extra measuring technique is needed to determine if, in case of doubt, intervention is necessary. Van Laar’s research elaborates on the work of two other TU/e doctors, dr.ir. Rik Vullings and dr.ir. Chris Peters. These engineers developed a way to measure a fetus’ heart rate using paste electrodes on the mother’s belly (Vullings), as well as software to analyze those signals (Peters).
Van Laar studied how to determine a fetus is in trouble based on their heart rate. It’s often paired with oxygen deficiency in the babies, which can be established by carefully sampling a drop of blood from a tiny incision in the head. She compared the heart rates of ten babies born with oxygen deficiency to those of ten healthy babies. The researcher has concluded it’s possible to determine whether or not the unborn child is really in danger by charting variations in heart rate frequency – to what extent the heart rate goes up and down as time progresses.
“The idea behind this approach is that variations in heart rate show us what part of the fetus’ nerve system, active or passive, has the upper hand. In case of relatively frequent slow variations, it means the active system is dominant, which is a sign the baby is stressed.” It may also be a sign the baby is just moving around, because that also triggers the active nerve system. “Looking at the heart of a marathon runner, one might conclude they’re stressed as well. It’s important to establish why the active nerve system is dominant, because it may not have a medical reason. Luckily, a fetus in distress has a tendency to lie still, and there are other ways to distinguish an active child from a baby in distress. Nonetheless, it is definitely something to keep in mind.”
As far as adults are concerned, we already know a lot about the relationship between heart rate variations and cardiovascular diseases, for example, but there´s only a handful of studies about unborn babies. It turns out it´s not easy to distill relevant parameters from their heart rate. The first thing you need to do, is do a so-called spectral analysis of the measuring signal, the well-known line moving up and down we know from countless hospital series. The analysis visualizes what frequency components are present in the heart beat (see figure).

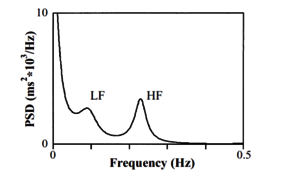
If the heart rate frequency fluctuates relatively slowly, a peak shows up in the left side of the graph. A high low-frequency peak means the baby is stressed, it turns out. Still, it only shows if you correct the readings for the mean heart rate, says Van Laar. “That has proven extremely important. Since with a higher heart rate the frequency variation decreases automatically, you run the risk of relative changes being veiled.”
It’s a complicated story, which boils down to this: any valuable predictions about the baby’s health can be done based on normalized power spectra only. And any values calling for intervention depend on how far the fetus has developed by that point, too. “There’s a period during pregnancy, roughly between 30 and 34 weeks, in which we can’t do proper measurements yet, due to the electrically isolating sebum the fetus develops in that period.”
All in all, it will be a while before spectral analysis of the heart beat, measured from ‘the outside’ with electrodes on the mother’s belly, will have become a standard procedure. That doesn’t take away the fact that they’ve already come a long way, says Van Laar. “Back when I was taking measurements, only three percent of our non-invasive electrocardiograms was suitable for analysis. The mother’s heart rate, muscle contractions and uterus largely dominated the baby’s signal. By now, that percentage has risen to 44 percent.”
That improvement could mean the difference between an infeasible method and one that can actually be implemented, she admits. “Over the past years, there have hardly been any new publications on this subject. I think it’s owing to the fact you need a team consisting of both engineers and doctors for this type of research. A doctor couldn’t do it alone, but neither could an engineer. The cooperation between hospital and university just works really well for this subject. And if you ask me, I’d say that’s pretty unique.”



Discussion