
- Research
- 18/06/2019
Detecting pressure ulcers in sweat and sebum
Pressure ulcers are a major burden to patients, carers and the healthcare system. Particularly vulnerable populations are elderly, bedridden and spinal cord injured individuals. PhD researcher Jibbe Soetens of TU/e investigated the response of the human skin to prolonged loading. Hospitals can use his results to detect and even predict pressure ulcers.
Prolonged loading on the skin can cause pressure ulcers. The loading leads to tissue deformation, causing local injury to the skin or underlying tissue. Current preventive methods are based on risk assessment and periodic control. However, these methods are subjective and there is a great need for more objective tools. Soetens discovered a set of indicators that enable early detection of pressure ulcer development. The set consists of metabolic and inflammatory biomarkers, of which the latter even have the potential to identify patients at risk.
Early detection
In order to survive prolonged loading, cells in the tissue must switch to anaerobic metabolism. The tissue also becomes inflamed. Soetens wanted to investigate whether these two reactions are measurable on the skin. He subjected a group of healthy volunteers to controlled loading of the sacrum, the largest vertebra, which is prone to pressure ulcer development. He then monitored the release of metabolic and inflammatory biomarkers, obtained from sweat and sebum on the skin surface.
Anaerobic metabolism appears to be visible at the skin tissue via lactate and pyruvate. Inflamed skin tissue is detectable via cytokine IL-1α. These indicators are therefore suitable biomarkers for early detection of tissue damage. Cytokine IL-1α even appears to be able to identify potential patients at risk, because a certain group of patients showed an increased response from this biomarker. These results potentially enable the clinical implementation of these biomarkers as an indicator for pressure ulcers.
In addition to clinical applications, the results can also be used to improve the design of preventive measures against pressure ulcers such as matrasses and wheelchairs. Currently their design is based on load distribution and periodic load relief. However, by focusing on the prevention of large internal deformations these measures will prove more effective.
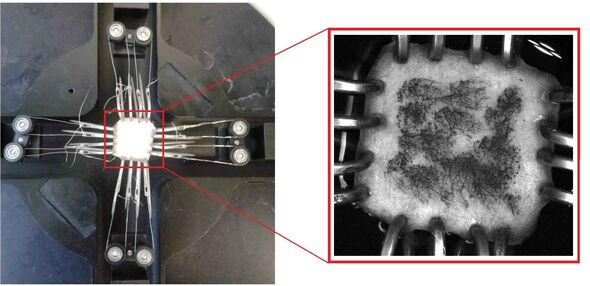
Read on below the image.
To improve the design, Soetens had to be able to accurately predict the mechanical response of the skin. That response varies greatly depending on the type of load. Soetens therefore developed a model based on mechanical experiments. Skin tissue was hereby subjected to a tensile load (see above). The model predicts skin deformations that may lead to the development of pressure ulcers. By using this model during the design of, for example, mattresses and wheelchairs, they can prevent pressure ulcers.
Jibbe Soetens carried out his research at the TU/e Department of Biomedical Engineering. He will be defending his PhD thesis 'Mechanical and biochemical response of human skin to diverse loading conditions' today, Tuesday June 18.
Discussion