Home Stretch | Predicting brain tumor growth
Benign brain tumors pose a dilemma for doctors: is it necessary to carry out a risky surgical procedure, or is radiation treatment the better option? Doctoral candidate Patrick Langenhuizen analyzed thousands of MRI scans of so-called vestibular schwannomas to answer that question.
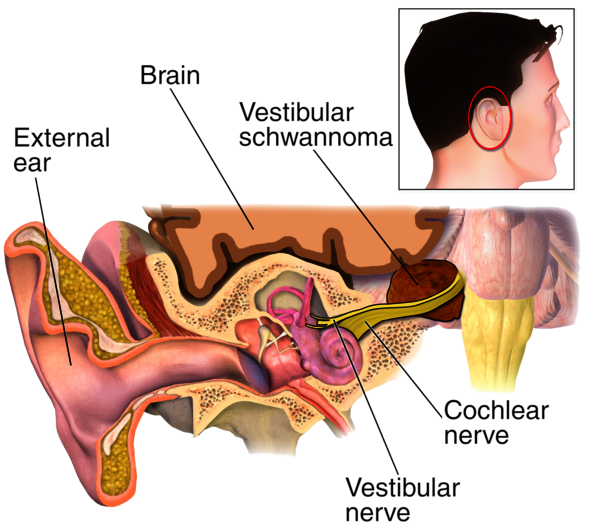
Vestibular schwannomas are tumors that originate from the outer sheath of the balance or hearing nerve, located in the cranial cavity behind the ear - between the brainstem and the cerebellum - known as the cerebellopontine angle. Although these rare tumors are benign, which means that they usually grow slowly over many years and don’t spread to other parts of the body, they can lead to hearing loss, tinnitus or balance disorders. If the tumor continues to grow, it will start to push on the brain and may even become life-threatening.
Radiotherapy
Vestibular schwannomas can be treated in two ways, doctoral candidate Patrick Langenhuizen explains. “The larger tumors are usually surgically removed; only partially in many cases, out of fear that it might lead to further nerve damage. An alternative treatment is radiotherapy with a so-called ‘gamma knife.’”
That machine, described as a radiation instrument with the accuracy of a scalpel, contains some two hundred radioactive sources, arranged in a hemispheric array so that the radiation from all those sources overlaps at one specific point only. “That allows you to target a tumor with precisely focused beams of radiation while sparing the surrounding tissue.” Ideally, the tumor will stop growing after one therapy.
The Elisabeth-TweeSteden Hospital (EZT) in Tilburg has been using a gamma knife since 2002; until recently it was the only hospital in the Netherlands with such a machine at its disposal. The EZT uses both a surgical approach and the gamma knife to treat vestibular schwannomas. In principle, radiation with the gamma knife is safer, less invasive and more cost-efficient than surgery, and is therefore the preferred option.
Unfortunately, little was known about which treatment works best in individual cases, Langenhuizen says. “There are hardly any studies on this, in part because these tumors are so rare.” That is why he, in collaboration with the Video Coding & Architectures group of professor Peter de With (TU/e department of Electrical Engineering) and neurosurgeon Jeroen Verheul, went to work at the ETZ to determine whether it’s possible to predict, based on MRI scans, the best treatment option for each individual patient.
Unique database
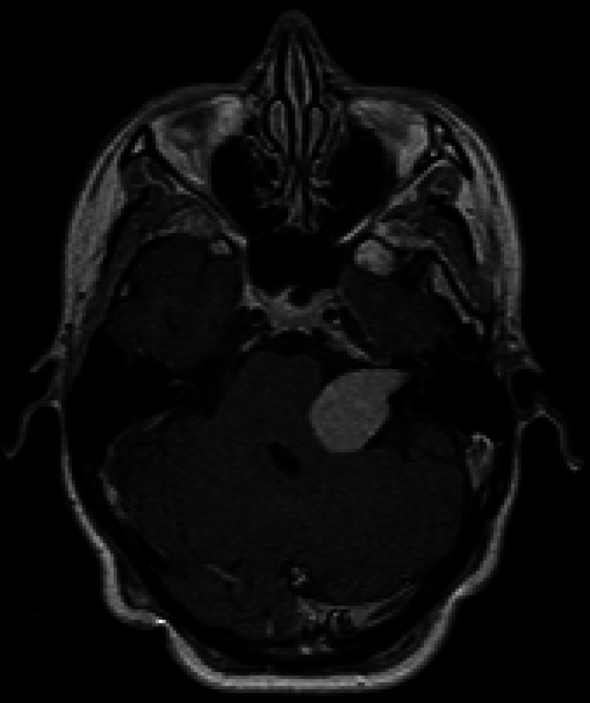
That quest started with drawing the contours of tumors in some four thousand 3D MRI images, from hundreds of patients who were treated in Tilburg - painstaking work that took him almost a year to complete. But it did provide him with a unique database that he could use for his analyses. “The MRI images of the tumor aren’t homogenous, instead they contain varying gray shades. The idea is that you can use artificial intelligence to find connections between such image characteristics and the tumor’s growth rate and posttreatment prognosis.”
One of the researcher's conclusions was that gamma knife radiation offers a slimmer chance of success when used for treatment of the fastest growing tumors. “It seems likely that a surgical approach is the best way to treat those tumors.” He also says that he can predict which tumors are likely to swell temporarily after radiation. “That occurs with approximately one in three tumors. If that happens with a large tumor that is already pressing against the brainstem, you will want to avoid that risk.” In addition, he is able to estimate which tumors will stay the same size in the long term, for a minimum of ten years after radiation treatment.
At the Video Coding & Architecture group, Langenhuizen is already building upon his doctoral research. As postdoc, he will supervise two doctoral candidates during the next four years. “The results from my project are very promising, but they still need to be validated with data from hospitals abroad where they apply the same radiation technique to treat vestibular schwannomas. And we’ll need to develop software for the models before doctors can start to use them.”


Discussion