
Home stretch | Better studies using virtual patient data
What if new medical treatments could be tested entirely on a computer—without involving a single human or animal? With his PhD research, Pjotr Hilhorst is taking the first step in that direction. The TU/e researcher develops computer models and uses data from “virtual patients” to improve medical diagnostics and predict the effectiveness of procedures and medications.
Pjotr Hilhorst’s PhD project is part of the European Horizon program In Silico World, which focuses on in silico clinical studies. “You have in vivo, which means research inside the body of a human or animal,” Hilhorst explains. “In vitro refers to research done in the lab, for example with cultivated tissues. And in silico means studies conducted on the computer—based on patient data and simulations.”
The project explores how in silico research can be integrated into real clinical workflows and addresses various aspects, ranging from legal frameworks to ethical questions. Hilhorst’s own work focuses on improving existing methods to enable more accurate computer simulations. Today, he defends his PhD thesis at the Department of Biomedical Engineering.
Simulations
Computer simulations can support precise diagnostics and help test the effectiveness of medical procedures and drugs. One major advantage is that they can reduce the need for animal testing and allow for smaller patient groups in clinical trials. Simulations also make it possible to test hypotheses in advance—before actual clinical trials begin—to get a sense of what outcomes to expect.
“It doesn’t guarantee that results will be identical in real life, but it does point you in the right direction,” says Hilhorst. “By conducting more targeted research, you can save both time and money—and avoid exposing patients to the risks of new procedures or medications.”
Narrowing arteries
In silico trials can, in principle, be applied to many types of medical research—from tuberculosis to bone fractures. For his PhD, Hilhorst focused on the cardiovascular domain, specifically the blood vessels. “Clinical studies on coronary artery disease were conducted at the Catharina Ziekenhuis in Eindhoven, and I tried to replicate those studies on the computer,” he explains.
“In coronary artery disease, the arteries narrow, which reduces blood flow behind the constriction—called a stenosis,” he continues. “Because less blood reaches that part of the heart, patients can develop angina pectoris: a painful or tight feeling in the chest caused by oxygen deficiency in the heart muscle. In the worst case, the artery can become completely blocked, leading to a heart attack.”
A clinical benchmark
When patients with chest pain arrive at the hospital, an angiogram is often performed. By injecting a contrast agent into the coronary arteries, doctors can visualize the blood vessels on an X-ray. “Based on those images, physicians assess how severe the narrowing is and decide whether an intervention is needed—but that’s quite subjective and not always accurate.”
To address this, the Catharina Ziekenhuis developed a method to measure pressure before and after a narrowing—a process that results in what’s known as the FFR value. “That gives a more objective picture,” says Hilhorst. “If the pressure ratio behind the stenosis is above 0.8, the narrowing can often be treated with medication; if it’s below that threshold, an intervention such as a stent is needed.” The method proved highly successful and is now used worldwide as a clinical standard. “We’re now investigating whether we can build models to predict this critical value—so that direct measurements aren’t always necessary. After all, those measurements carry some risks and are only done when absolutely needed.”
A virtual patient cohort
Unfortunately, the available clinical data from that study were often incomplete or inconsistent. “Our model had about 35 parameters, but for each patient we could only fill in 3 or 4. That wasn’t enough for proper simulations,” Hilhorst explains. “That’s just how things go in hospitals—medical staff’s first priority is helping patients, not gathering every data point for a model.”
To solve the data problem, Hilhorst generated a large amount of synthetic patient data to fill in the gaps. “We call that a synthetic virtual patient cohort. These aren’t real people, but they’re realistic representations,” he says. “We fed the model with a wide range of input values and filtered everything based on natural physiological boundaries, so the data remained realistic.” The model then calculated the FFR values, which were compared to those from real patients. The outcome? The simulated results matched the real-world data remarkably well.
A 3D structure
The next step was improving the model further. “A sensitivity analysis showed that we needed to better represent the shape of the narrowing,” Hilhorst says. “We noticed that the constrictions in our synthetic patient population always followed a perfect sine curve, while in real patients they’re much more irregular and varied.”
To make the synthetic data more representative, he incorporated 3D simulations of the narrowing into the model. “The more complex the model, the more computing power it requires—so it’s always a trade-off between speed and accuracy.” By integrating 3D structure into a simplified 1D model, the system can now run simulations within a few hours and produce more precise results.
Laying the groundwork
“Ultimately, these simulations should be repeated and the improved model re-evaluated. The input must keep improving until the virtual patient cohort truly reflects the real population,” Hilhorst says. He admits that it’s still a long road, with many measurements needed to validate and implement the model in practice. “But with my PhD project, I have laid the groundwork for how such a study can be conducted using a synthetic virtual patient cohort.”
PhD in the picture
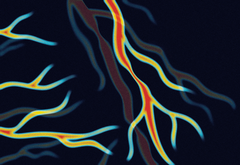
What’s on the cover of your PhD thesis?
“It’s an abstract depiction of coronary arteries, with a suggestion of multiple narrowings.”
You’re at a birthday party — how do you explain your research in one sentence?
“I study how we can simulate a patient’s blood circulation so that clinical research can be done on a computer.”
How do you unwind outside of your research?
“I’m an avid Dungeons & Dragons player (a tabletop fantasy role-playing game, ed.). I also love dancing, working out, and gaming.”
What piece of advice do you wish you’d received at the start of your PhD?
“Your supervisors are the most important factor—they can make or break your experience. Make sure they’re a good match and that you have a strong connection. Of course, luck also plays a role. I was fortunate to have the perfect supervisors, which made the entire PhD period really enjoyable and relaxed.”
What’s your next chapter?
“I’m starting as a system integrator at Philips Healthcare in Best. My department focuses on CT scans, which are used, among other things, for imaging coronary arteries in hospitals. After four years of technical research, this new role is much more social and involves less time behind a computer—and I’m ready for that change.”

Discussion