
Home Stretch | Bare ACL grafts for a stronger knee
A new type of cruciate ligament graft reduces complications and shortens rehabilitation period
It’s every top athlete’s worst nightmare: an anterior cruciate ligament injury. TU/e researcher Janne Spierings developed a new protocol for cruciate ligament grafts that should reduce complications. Monday, she will defend her dissertation at the Department of Biomedical Engineering.
For every presentation she gives, PhD candidate Janne Spierings cites a recent example from the list of top athletes with cruciate ligament injuries. “Last time, it was Bayern Munich’s key player Alphonso Davies. The Canadian professional soccer player came back injured from an international match with the national team this spring: a torn ACL in his right knee, and out of play for at least six months. He celebrated Bayern’s league title on crutches.”
We’re given a brief anatomy lesson. The anterior cruciate ligament (ACL) is located in the center of the knee joint and provides stability to the knee. The ACL prevents the lower leg from rotating too far in relation to the upper leg. As such, the ACL plays an important stabilizing role, especially during twisting movements or sudden changes in direction.
Crack or pop
And that is exactly why so many (professional) soccer players, hockey players and handball players suffer injuries to this tendon, Spierings explains. “Rapid twisting and cutting movements put a lot of force on the knee joint, and if those forces become too great, a cruciate ligament can tear.” That happens in the blink of an eye, she emphasizes. “In about 45 milliseconds, there’s a crack or a pop, followed by pain.”
Because tendons and ligaments have limited blood flow – with less supply of nutrients and slower removal of waste substances – recovery often takes a long time. In the case of an ACL injury, the cruciate ligament is often surgically replaced with a new tendon, which usually comes from the patient’s own hamstring or patellar tendon. Afterwards, this tendon has to adapt to its role as a new cruciate ligament by remodeling. A lengthy process, and there is no guarantee that the knee will be able to bear full weight again.
Unfortunately, ACL reconstructions often come with numerous complications, says Spierings. “The strength of the graft decreases significantly after reconstruction, increasing the chance of re-tearing the ACL. And almost half of the patients develop early-onset osteoarthritis. That’s something you tend to associate with elderly people, but here it usually affects very young people instead.”
Movement simulations
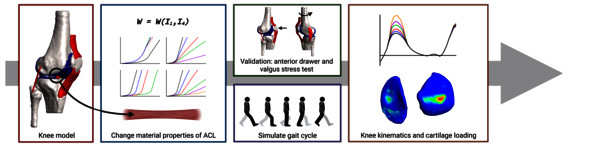
Using a “simple” computer model, Spierings tried to determine the cause of this early-onset osteoarthritis. “We wanted to study the mechanical properties of the graft in isolation: what happens when its strength deteriorates? This causes two movements associated with the ACL to increase, resulting in a greater range of motion for the entire knee.” In simulations, Spierings saw that this has consequences for the contact pressure on the underlying cartilage. The damage caused by this could potentially trigger the onset of osteoarthritis.
And so, Spierings turned her attention to limiting the loss of strength in the graft. She developed a protocol for a decellularized – “bare” – graft. “The new ACL contains all kinds of cells that provide strength. But when the piece of tendon is briefly removed from the body to be “folded to size”, these cells die. When this happens, they release signaling proteins that can trigger an immune response. Immune cells then start breaking down the tissue like little Pac-Men, which can cause extra damage and loss of strength.”
Stretching and extending
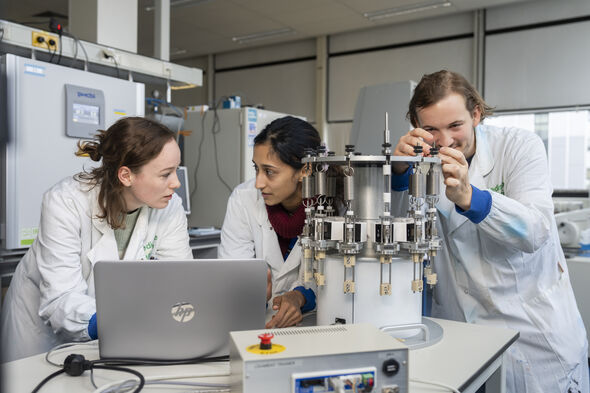
In collaboration with the Maxima Medical Center, Spierings was able to use leftover pieces of cruciate ligament grafts to optimize the washing protocol and study its effects. She also used a bioreactor for this purpose, so that she could cultivate the tendons in a dynamic way.
This proved successful. “We had previously designed this machine with incredible help from the Equipment and Prototype Center. Twelve tendons can now be cultivated at the same time, while they are continuously stretched and extended. Thanks this model, fewer animal tests are needed for improving ACL grafts. A very positive development that’s gaining traction within TU/e.”
The washed grafts proved to be a good substrate for new cells to attach and grow. In her cultivation model, Spierings even observed the first signs of so-called cell infiltration. These are promising initial results, but clinical application is still a long way off, she cautions. “We spend two days washing the grafts to get them decellularized. That needs to be done much faster, of course.”
Fewer crutches, more strength
Spierings can now also simulate the first few weeks after an ACL surgery in the bioreactor. She has already conducted several pilot experiments to measure which signaling substances are released by dying cells. This can be used to investigate how those substances could trigger postoperative complications, and her colleagues will focus on finding a biomarker for personalized rehabilitation. Memphis Depay, Estavana Polmann, and Alphonso Davies can no longer benefit from this. However, for all future ACL patients, Spierings hopes that the bare grafts will ultimately lead to “fewer crutches and more strength.”
PhD in the Picture
What is that on the cover of your dissertation?
“It’s a failed experiment, actually. Under the microscope, I suddenly saw both a cross-section and a longitudinal section of the cruciate ligament. Circles and stripes, a beautiful image. That failure suddenly turned into something positive.”
You’re at a birthday party. How do you explain your research in one sentence?
“I look at how we can reduce complications associated with ACL surgery.” Spierings continues with a laugh: “And then the stories start. Pretty much everyone knows someone with a torn ACL; I’ve been given a great deal of medical details over the past few years. But I always tell them: ‘I’m not a doctor’.”
How do you blow off steam outside of your research?
“I exercise a lot. I highly recommend the group classes at the SSC. And the more frustration, the better the workout.”
What tip would you have liked to receive as a beginning PhD candidate?
“Don’t let a PhD take over your whole life; relaxing is also very important. Of course, it’s hard work. And sometimes that means working evenings or weekends, but that shouldn’t be the norm. Protect your personal time. I think supervisors should encourage that too.”
What is your next chapter?
“With summer just around the corner, I’m going to enjoy my vacation first. And then I’ll think about what I’m going to do next. Over the past four years, I’ve come to realize that the academic world is not the environment I want to continue in. I think many things could and should be done differently, and those issues can’t be solved in just a few months. So I’d rather not be part of that.”

Discussion